Chronic Stress After Traumatic Brain Injury TBI
- Power Of Patients
- May 20, 2023
- 5 min read
The Brain’s Response to a TBI
Sustaining a traumatic brain injury is a shock, not just on your brain, but your entire body. In an unstable environment, the body has to adapt continually. The body copes with this pressure by triggering a long-term, chronic stress response. This process accumulates over time, described by the allostatic load theory coined by cell biologist McEwen in 1993. Allostasis is a regulatory process that responds to stressors, as opposed to homeostasis, which is where the body maintains its current balance. McEwen’s theory asserts that exposure to stress leads to a "wear and tear on the body.” [8]
Natural selection increases the frequency of adapting traits that help us survive and reproduce in our environment. In this vein, the stress response evolved to maximize chances of survival in the face of imminent danger, like a big animal. The “fight or flight” response is triggered by hormones that increase energy supply and shut down non-essential functions. However, the “stress hormone” cortisol can wreak havoc on your body. Cortisol, although an anti-inflammatory protein, actually triggers a cytokine storm, an acute pro-inflammatory response. Chronic inflammation heightens the risk for diseases including heart disease, diabetes, cancer, and arthritis. [6]
The brain is an energy-demanding organ. Despite only comprising 2 percent of our body mass, our brains consume 20 percent of the body's oxygen supply. Tissues need oxygen and glucose to make the energy they can consume. Different parts of the brain suffer during the stress response. Cortisol mediates the delivery of glucose. However, it prioritizes getting energy to tissues involved in essential tasks, including breathing, temperature, hunger, rather than areas in the brain responsible for executive functioning. Consequently, the hippocampus, responsible for learning and memories, and the prefrontal cortex, capable of decision making, have diminished activity. [7]
The brain under stress:
Hippocampus and prefrontal cortex activity decrease while the amygdala is overactivated.

Chronic stress leads to overactivation of the hypothalamic-pituitary-adrenal (HPA) axis, causing hormone overproduction. The HPA pathway perpetuates a cycle for the stress response since cortisol activates the production of more cortisol. The center of this stress response is the amygdala known as the “fear promoting region”. The amygdala is normally responsible for emotional regulation, and in a stress response, it heightens feelings of anxiety. [3]
After a TBI, there is widespread neuronal death. To compensate there is a proinflammatory and excessive activation of the HPA axis. Accordingly, excessive cortisol is released, inducing microglial priming and increasing inflammatory cytokines. The increased reactivity and hormone activation lead directly to the stress response. [1]

The brain’s fear response: A stressor, symbolized as a bear, violent person, or electric shock the brain structures involved in the fear response causing the possible behavioral outcomes to the fear [5]
Integrating Chronic Stress and TBI
Looking at TBI from the perspective of the chronic stress response can help identify new drugs and treatment strategies that can manage TBI symptoms. It could also help identify how stress could exacerbate TBI prognosis and development.
A 2017 study published in the Proceedings of the National Academy of Sciences found that a drug that was used to inhibit the integrated stress response (ISR) was also effective at mitigating the cognitive deficits of TBI in mice. The mice had induced TBI in the right parietal lobe and experienced phosphorylation (activation) of a protein that transcribes immunological genes. The ISR drug prevents the activation of these genes which result in an overactive immune response. Other drug mechanisms include the regulation of cortisol to prevent inflammation to tissues and damage to the brain [2].
Schematic from Chronic Stress and Fatigue-Related Quality of Life [2].

Describes how social determinants of health and TBI injury affect chronic stress. Both psychological stress and PTSD impact fatigue-related quality of life.
The Journal of Head Trauma Rehabilitation published a study in 2011 that monitored mild to moderate post-TBI patients [3]. Chronic situational stress was associated with higher self-reported levels of fatigue. The symptom of fatigue supports the theory that TBI impacts chronic situational stress as well as event-related stress.
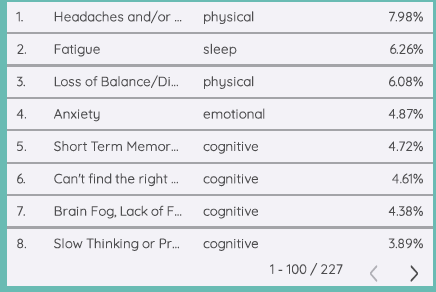
It is clear from our Power of Patients data warehouse that our users struggle with sleep, as fatigue is the second-highest medical symptom tracked, following closely to heads and/or migraines. As mentioned above, being able to recognize that you may not be receiving enough sleep could be the first step to improving your overall quality of life.
Pulled from Power of Patients Data Warehouse
Event-related stress is typified by post-traumatic stress disorder (PTSD) and is caused by a triggering event. The memory of the event is a source of anxiety or depression. Natalie Becker, who has sustained a TBI, recounted her experience, “When my injury was still fresh, I was very sensitive and often scared. I was often experiencing PTSD in simple, daily tasks.” PTSD is associated with structural changes in the brain, so its symptoms are likely triggered by brain dysfunction. However, PTSD does not act in the exact mechanism of chronic stress.
Tracing the level of cortisol is a valuable way to assess the impact of TBI and PTSD. Cortisol is overactivated in TBI. The HPA has suppressed activity in PTSD, corresponding to less variable and lower amounts of cortisol for PTSD patients throughout the day. However, during exposure to a stressor, PTSD has a spike in cortisol levels. For people who have a TBI and PTSD, their combination leads to a variance of cortisol [9].
To fully understand post-TBI pathology, it is important the stress response be seen as a parallel and intertwining phenomenon. Often people sustain a TBI during a car crash, gun injury, or assault, which are in themselves stressors that can trigger PTSD. The chronic stress response is often overlooked but can provide an explanation and starting point to treat TBI symptoms [4]. As one article states, it is essential for “future research to better define the role of stress-immune pathways in mediating outcome following TBI [1]”.
How Power of Patients can Help
The Power of Patients Dashboard, Sallie®, allows brain injury survivors and caregivers to track symptoms daily, with the ability to rate the severity and add descriptions of the event and coping strategy used. This allows patients to understand what is happening to them and advocate for care for themselves. This is particularly important for individuals trying to overcome PTSD, our journalling space allows them to express themselves and to note triggers that caused them to have a PTSD flashback.
As mentioned, Sallie® can track your stress triggers and symptoms easily and they are automatically compiled into one place. At any point in the day when a stressor or trigger is affecting you, you can quickly log into Sallie® and track how you are feeling. A personalized data report is generated so you can easily see what seems to affect you and when.
Power of Patients understands that brain injury survivors not only deal with symptoms following their brain injuries, but stressors within their homes, communities, and societies that compound these symptoms and worsen their physical and mental states. We endeavor to support and advocate for brain injury survivors and their caregivers. Sign up for our free symptom and trigger-tracking Dashboard at powerofpatients.com to start identifying your stress triggers and taking back control of your life, today!

Comments